As breast cancer cases rise among Indian women, awareness and early diagnosis are critical. Here’s a look at key challenges, common myths, and the importance of empathy in treatment
October is observed as Breast Cancer Awareness Month, a time to make a concerted effort to raise awareness, show support, and enhance survival rates. Breast cancer remains the most common cancer in women and is a curable cancer with early detection and proper treatment.
This year’s theme is “Every story is unique, every journey matters.”
It highlights how every patient’s journey with the disease — from diagnosis to treatment and rehabilitation — is personal and different, and the need for compassionate, timely, and quality care for all.
Q1. As a female oncologist, what do you think are the major challenges in breast cancer treatment in India?
Mainly late-stage diagnosis, lack of resources or accessibility for screening and treatment, and lack of awareness about symptoms. But one of the major issues is the cultural stigma that really pulls women back from coming forward with symptoms. Widespread myths about the disease also hamper the situation.
Q2. Can you highlight some common myths about breast cancer?
Commonly, people think either that all breast lumps are cancerous or that any lump without pain is not problematic. Other myths include that only older women get cancer, that wearing a bra (underwired or otherwise) can cause cancer, or that using deodorants or talc can cause cancer.
Some believe mammography is painful and harmful, that all breast cancers are hereditary, or that doing a biopsy can spread the cancer. These are all myths.
Q3. What are the common symptoms of breast cancer?
-
Lump in the breast (painless or otherwise)
-
Nipple retraction
-
Change in the skin
-
Bloody or other discharge from the nipple
-
Lump in the armpit or neck
Q4. How does being a female oncologist help change your approach to breast cancer patients?
Firstly, it helps in getting patients to come for check-ups. With our society still treating it as a “women’s disease,” women feel more comfortable getting examined and openly discussing their complaints. The feeling of security and understanding is better.
Secondly, certain aspects of breast cancer treatment — like surgery (removing a body part) or hair loss during chemotherapy, which create changes in self-image — can be better empathised with by a female oncologist.
Q5. What are the psychological aspects of the disease, and how can they be dealt with?
Psychological aspects such as anxiety and fear are often overlooked in our system — both by doctors and family members.
Fear of the disease, anxiety about treatment side effects, permanent alterations in body image, and the stress of living with the disease — especially in advanced cases — are all relevant and common situations we face.
These issues can be managed through:
-
Breathing exercises
-
Yoga and meditation
-
Counselling sessions
-
Spending quality time with the patient
Q6. Breast cancer is being seen more and more in young women nowadays.
There are various hereditary factors, such as BRCA mutations, and environmental factors like obesity, hormonal exposure, and alcohol intake, which have increased the incidence in younger women.
This form of cancer is often more aggressive.
An important issue that arises with younger women is fertility preservation, as many cancer treatments can reduce the chances of having children later in life.
Q7. What is your message for women this month?
All I wish to emphasise to women this month is to take charge of your own health and not live in fear.
Breast cancer is a curable disease when detected early, and many advanced treatments — including targeted therapy, immunotherapy, and breast-preserving surgery — are now available.
Q8. What are the options for early detection?
Early detection plays a key role in saving lives. Recommended steps include:
-
Self-breast examination every month
-
Clinical breast examination every six months by a doctor
-
Yearly screening mammography for women above 40 years
Q9. What can we do as a society to improve breast cancer care?
As a society, we can make a difference by:
-
Providing women with a safe space to share symptoms and stories
-
Organising awareness events in communities and workplaces
-
Conducting screening camps
-
Supporting local organisations through volunteering and donations
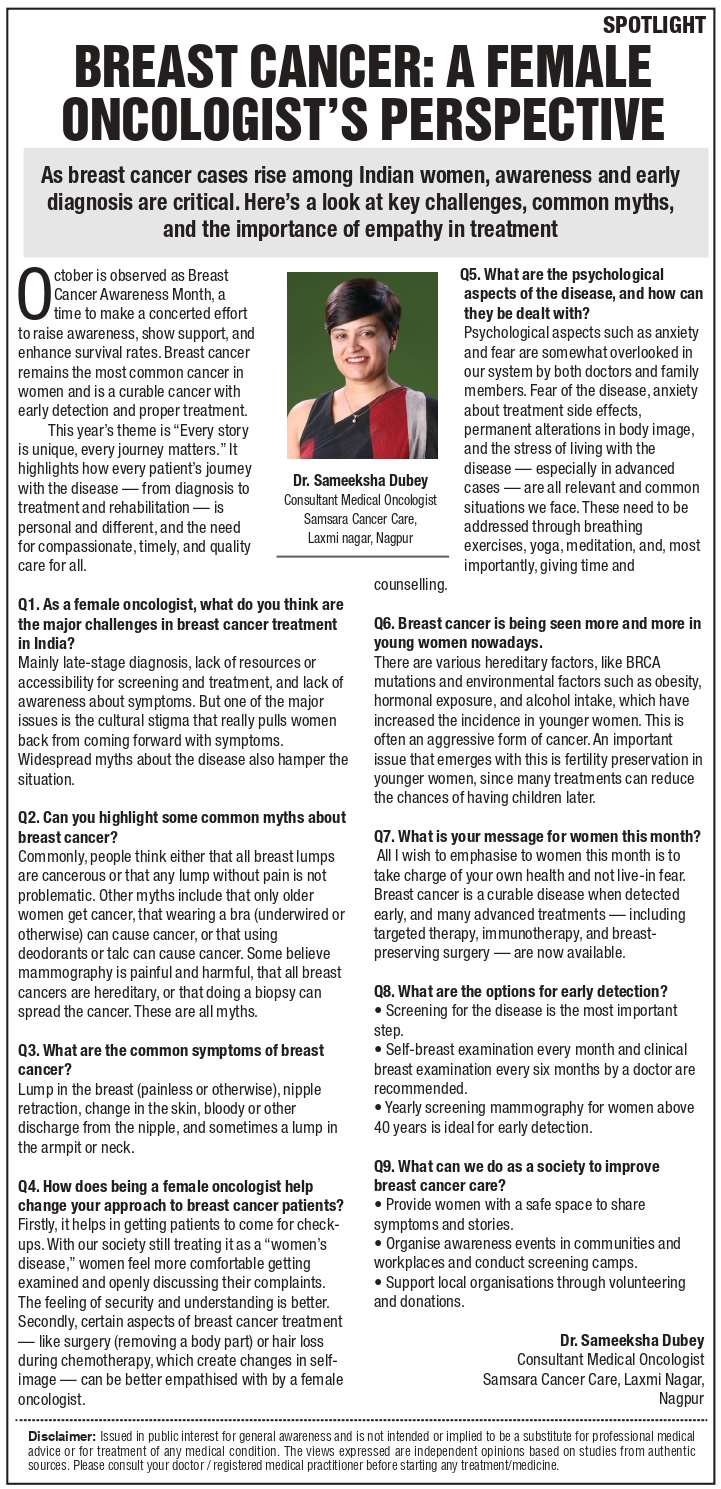
Dr. Sameeksha Dubey
Consultant Medical Oncologist
Samsara Cancer Care, Laxmi Nagar, Nagpur