Introduction to Cervical Cancer
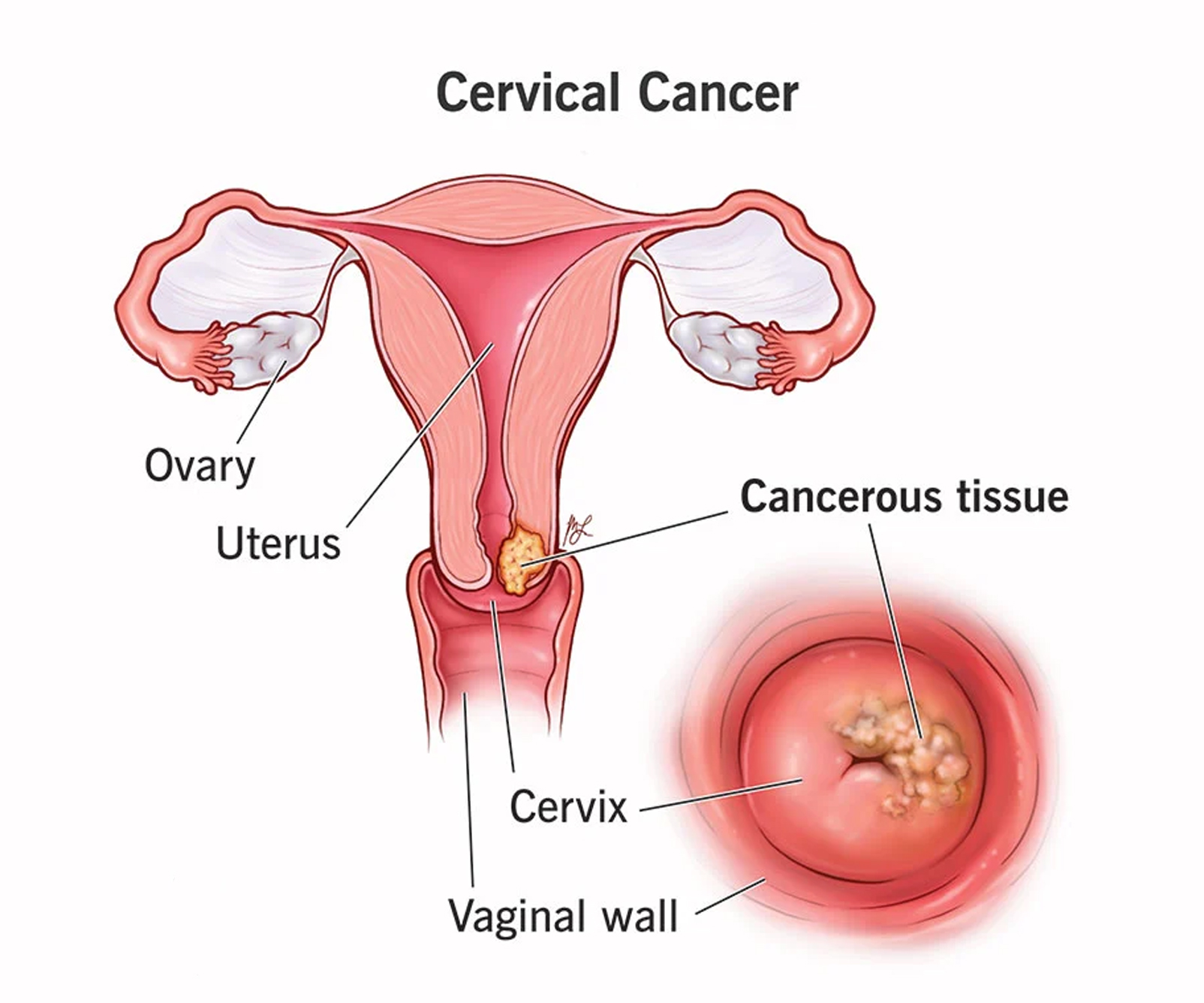
Cervical cancer primarily affects the cervix, the lower part of the uterus. It is one of the most common cancers diagnosed in females. Human papillomavirus (HPV) infection is the primary cause, and certain strains of HPV are linked to the development of cervical cancer. It is a preventable cancer through health education and screening programmes. Successfully done cervical cancer treatment in Nagpur
Prevalence in India
Cervical cancer is a leading cause of cancer-related deaths among women in India. An estimate states that approximately 1,25,000 new cases of cervix cancers are diagnosed in India every year. Factors contributing to its prevalence include inadequate healthcare access, lack of awareness, and limited screening programs in many regions. According to statistics, India accounts for a significant portion of the global burden of cervical cancer cases.
Risk Factors
Various factors contribute to the risk of developing cervical cancer, including:
HPV Infection: Certain strains of HPV, especially HPV-16 and HPV-18, significantly increase the risk.
Lack of Screening: Women who have not undergone regular cervical cancer screening are at higher risk.
Smoking: Tobacco use increases the risk of cervical cancer.
Weak Immune System: Individuals with weakened immune systems due to HIV/AIDS or immunosuppressive medications are at higher risk.
Early Sexual Activity: Engaging in sexual activity at an early age increases susceptibility.
Multiple sexual partners and early/ frequent births: can increase the risk of cervical cancer.
Symptoms
Early stages of cervical cancer might not display noticeable symptoms, but can present with abnormal vaginal bleeding, which can be post intercourse, inter menstrual or post menopausal. Another symptom includes abnormal vaginal discharge which can be blood stained, dirty, whitish or foul smelling.
As it progresses, symptoms may include pelvic pain, pain during sexual intercourse, and symptoms related to urination ( difficulty in passing urine or blood discharge) or difficulty in passing motions.
Diagnosis
Cervicalervical cancer diagnosis involves a careful examination of clinical signs and specific procedures to confirm andstage the disease. Understanding these steps is crucial for timely intervention and treatment planning.
Clinical Signs:
➤ Abnormal growth, ulcer, or irregular area on the cervix
➤ Induration (hardening)
➤ Friability (tendency to bleed easily)
➤ Bleeding upon touch
➤ Fixity (immobility or stiffness)
Confirmation of Diagnosis:
Biopsy: Essential for confirmation from obvious growth or abnormal area directed biopsy for very early lesions Cone biopsy for precise analysis
Staging Procedures:
➤ intravenous Urography
➤ Abdominal Ultrasonography
➤ Cystoscopy
➤ Proctosigmoidoscopy
➤ Examination Under Anesthesia (EUA)
➤ CT/MRI imaging for detailed assessment
Baseline Investigations:
Assessing general condition to determine overall health status
Screening
Common Screening Methods in India
In India, screening methods such as Pap smear tests, HPV DNA tests, and visual inspection with acetic acid (VIA) are commonly used. Efforts to improve screening programs have been made, but accessibility remains a challenge in rural and underserved areas.
➤ ACS/USPTF Screening Recommendations
➤ Women Under 21 Years: Screening is not recommended.
➤ Women Ages 21 to 29 Years:
➤ Pap smear every 3 years.
➤ HPV test if the Pap smear shows abnormal results.
➤ Women Ages 30 and Above:
➤ Preferred method: Pap smear along with HPV testing (co-testing) every 5 years until the age of 65 years.
➤ Alternative option: Pap smear every 3 years.
➤ Women aged 66 and above, with regular screening in the past 10 years showing negative results, can discontinue screening.
Exceptions:
➤ Total hysterectomy (removal of the uterus and cervix) indicates stopping screening unless done for cervical pre-cancer or cancer.
➤ Hysterectomy without cervix removal requires continued cervical cancer screening as per guidelines.
➤ High-risk individuals may need more frequent screenings based on their doctor’s recommendations.
➤ Women vaccinated against HPV should adhere to age-appropriate screening recommendations.
➤ Screening Frequency: Avoid yearly screening for women of any age by any method.
Prevention
HPV vaccination significantly reduces the risk of cervical cancer, but its accessibility and affordability in India are limited.
Vaccination Schedule:
➤ Girls 9 through 14 years: Two doses to be administered at an interval of 6 months, 0–6 months.
➤ Girls 15 years and older: Three doses recommended in the schedule 0–1–6 months for Cervarix and 0–2–6 months for Gardasil.
➤ In immunocompromised individuals of any age: Three doses recommended in the schedule 0–1–6 months for Cervarix and 0–2–6 months for the Gardasil.
➤ HPV9 is licensed in a 3-dose schedule of 0-2-6 months in females 9-26 years of age and males 9-15 years of age.
➤ The ideal age for starting the vaccine is 9-10 years. HPV vaccines can be given at the same time as the Tdap vaccine.
Why is it essential to start the schedule at 9-10 years and not later?
1. Young adolescents mount a superior immune response compared to older individuals.
2. Prevention of disease is better if started earlier
3. Only 2 doses are necessary in this age group versus 3 doses beyond 15 years of age. There is no recommendation for any booster doses.
These vaccines are generally safe. Mild to moderate local side effects are pain, swelling or redness at the vaccine site. Some adolescents may have giddiness or fainting sensation after the shot. It can be minimized by giving the vaccine in a lying down or reclining position. All the patients should be monitored for at least 20 minutes for any immediate side effects.
All girls (>9 years) and adolescent girls should receive this vaccine. Catch-up vaccination may be offered to older women till 45 years. Vaccination of males will offer some protection against other HPV related cancers penis, anus and oropharynx (mouth and throat). In India, only the HPV 9 vaccine is licensed in males.
Regular Screening
Encouraging regular Pap smears or HPV tests is vital as they can detect precancerous changes early, aiding in timely intervention.
Safe Sex Practices
- Practising safe sex and limiting the number of sexual partners can significantly reduce the risk of HPV infection. This includes:
Avoiding early marriage and intercourse
Promoting hygiene practices
Using barrier contraception methods
Treatment Options
Treatment varies based on factors like cancer stage, patient’s age, tumor type, and overall health. Options may involve surgery, radiation therapy, chemotherapy, or a combination. However, comprehensive cancer treatment facilities in India vary across regions.
Challenges in India
Awareness and Education:
Lack of awareness about cervical cancer, its causes, and preventive measures.
Access to Healthcare:
Rural areas often lack proper healthcare infrastructure and screening facilities.
Vaccination Access:
The HPV vaccine is not yet part of the national government immunization schedule in India. While recommended by NTAGI, the inclusion process began recently. Currently, obtaining the vaccine involves purchasing it, with costs ranging from 3000 rs to 11,000 rs per dose.
Stigma:
Social stigma around discussions related to reproductive health and cancer can hinder early detection and treatment-seeking behavior.
Initiatives and Progress
Efforts have been made in India to combat cervical cancer
Government Programs: Initiatives like the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS) aim to improve cancer screening and treatment.
NGO and Public-Private Partnerships: Collaborations to increase awareness, vaccination drives, and screening programs in remote areas.
For more information and consult meet Dr. Sameeksha Dubey, oncologist known for best cervical cancer treatment in Nagpur. experience and commitment to advancing cancer treatment
